If any of you would like to know the originating story, you can follow this Our Story
But the purpose of this post is to give all of you a sense of the future of Healthcare that we are building for 1.2 billion Bhartiya (excluding the top 10% of India’s population). Also, we want to build this future in a way that could be sustainable for all the stakeholders including the environment. And by posting here, we will get feedback from all of you.
We can understand the problem in four and five points:
- India’s healthcare expenditure per capita is INR 5020 extremely lower than USA’s INR 8,76,838 and China’s INR 42,800. This means healthcare is unaffordable to the masses in all three countries - India, the USA, and China (this is true for the rest of the world).
- And hence unaffordability of Healthcare is not just India’s problem but a global problem.
- USA, China, and the rest of the developed countries solved the unaffordability of healthcare costs and made healthcare universal using the tool - Health Insurance.
- 95% of the USA and China’s population are insured under Health Insurance. In India, less than 10% of the population is insured under Private Volunteer Health Insurance (PVHI). This is because the available Health insurance is unsuitable, unaffordable, and unattractive for 90% of the population.
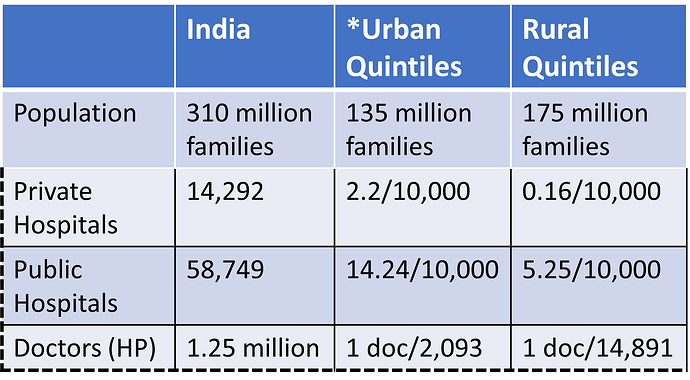
- Unsuitable because of the uneven distribution of Healthcare supply: here is a picture of the current healthcare supply distribution
The super uneven supply distribution force 90% of India’s population to travel 3 or 4 times up to 1000 km for decent treatment and diagnosis. And travelling costs also have been an obstacle for women to access healthcare.
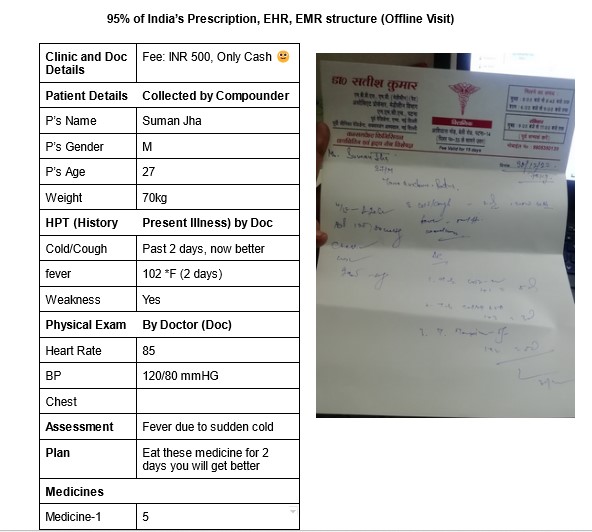
- Unattractive because available Health insurance only covers IPD (Inside Patient Department) expenses but 70% of Healthcare expenditures are on OPD (Out Patient Department). This makes the available Health insurance unattractive and hence zero motivation to pay - cutting present cost for an uncertain future risk is not attractive.
- Unaffordable because there is no underlying technology that can measure the health insurance premium based on individual profiles. The current method is one size fits all - adverse risk polling: insurance companies offset their losses of sick people (higher risk) by charging more from healthy people (low risk).
You see, it would be impossible to build or transfer Healthcare infrastructure evenly because it will demand billions of dollars of investment and that will further inflate Healthcare costs.
This leaves us with just one option build a Coordinated and integrated Healthcare infrastructure using available resources and technology. Frankly, just a few years back thinking about solving this problem would have been foolish thoughts. But thanks to multiple forces, today it is possible to solve this problem.
What are those forces:
- Health stack: ABDM (Ayushman Bharat Digital Mission)
- Partially-trained Health Professionals - ASHA, AW, CHO etc
- Technological leapfrog on the AI front - if the current AGI is a child and utilized with moral responsibility has tremendous potential to solve many of our complex problems.
With all these forces and keeping the affordability for consumers in the centres, we have come up with a solution that has real potential to make healthcare universal in India.
We are also extremely excited about the solution’s potential to create 10 million female local jobs that have the potential to create a strong flywheel in making healthcare universal in India.
How?
India has 4 million semi-skilled women health professionals who are, based on their Impact, the spine of India’s primary healthcare, do most of the heavy lifting and have a strong personal connection with the local community - the custodian of hyperlocal trust. And with little effort and the right technology we can convert them into skilled health professionals that can be integrated into a coordinated and integrated healthcare infrastructure. And generate enough work for them so they could employ two more employees and boom - we have 10 million local jobs that would be making healthcare affordable for 1.2 billion Bhartiya. The work on this has already got started!
How much Co2 and travelling costs of consumers it can save?
National Health Profile 2021 released by the Central Bureau of Health Intelligence (CBHI), there were a total of 1.1 crores (11 million) admissions in the year 2019-20 in India, which works out to be an average of approximately 30,000 admissions per day.
- Let’s say 80% of such admissions demand 3 or 4 travels - we can settle with 3 travels and an average distance of 100KM
- Total Hospital admission by 80% of the population = 1.1*.8 = 88 Lakhs
- Number of travel = 88*3 = 264 Lakhs (2.64 Crores)
- Total distance travelled per year = 2.64*100 = 264 Cr KM
- Let’s consider these buses are run on diesel = 7KM per litre
- Fuel require to cover 264 Cr KM = 264/7 = 37. 71 Cr Litre
- Let’s consider fuel price INR 100/litre and hence fuel cost = 37.71*100 = 3771 Cr
- Co2 release per litre of diesel (There are other gases SoX, Nox etc)= 2.68 KG
- Total CO2 release = 37.71 Cr * 2.68 KG = 101.062 Cr KG of CO2
This means we can save 101.062 KG of Co2 emission and INR 3771 Cr of travelling costs per year by building coordinated and integrated healthcare for 1.2 billion Bhartiya. What we all need to understand is that these are from 2019-20, the new numbers would be much higher.
Note: This is inevitable that the Healthcare expenditure per capita is going to rise and in that case, scale is one of the tools that will make healthcare affordable for 1.2 billion Bhartiya. For example, an INR 2 Lakhs of IPD health insurance is possible for a premium under INR 200 provided the number of risk polls is 10 Cr (100 million). And this amount would be affordable for every single Indian.
Note 2: There is tremendous power in standardization and scaling a product among 90% of the Bhartiya. Here is one example: In the 5 years 10 Cr+ (100 million+) consumers have enrolled for term insurance for a claim amount of just INR 2 Lakhs.

And we understand those channels that can be utilized to scale the Jile Health solution.
I would love to hear feedback from all of you and answer your queries!